The Afferent Arteriole: The Gatekeeper of the Kidney
What is the Afferent Arteriole and Where is it Located?
To understand the afferent arteriole, we first need to look at the kidney's microscopic functional unit: the nephron. Each kidney contains about one million nephrons, and each one is a sophisticated blood-filtering factory.
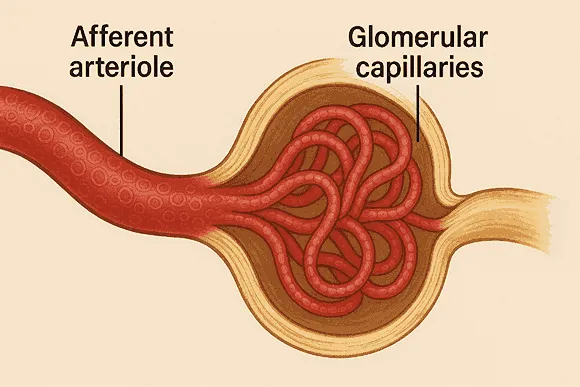
Imagine a single nephron as a complex, tiny tube. The process begins at a structure called the renal corpuscle, which looks like a ball squeezed into a round cup. The afferent arteriole is the small artery that delivers blood to this ball of capillaries, known as the glomerulus. The word "afferent" comes from Latin, meaning "to carry toward." After the blood is filtered, it leaves the glomerulus through another small artery called the efferent arteriole ("efferent" meaning "to carry away").
So, the path is: Afferent Arteriole → Glomerulus (Capillary Ball) → Efferent Arteriole.
| Feature | Afferent Arteriole | Efferent Arteriole |
|---|---|---|
| Function | Brings blood into the glomerulus | Carries blood away from the glomerulus |
| Diameter | Larger (under normal conditions) | Smaller |
| Blood Pressure | Higher pressure as it enters | Lower pressure as it exits |
| Analogy | The main water pipe feeding a filter | The narrower pipe draining the filter |
The Physics of Filtration: How the Afferent Arteriole Creates Pressure
The primary job of the glomerulus is to filter the blood, pushing water and small dissolved substances (like salts, glucose, and urea) out of the bloodstream and into the nephron tubule. This process is called glomerular filtration. For this to happen, there needs to be enough pressure inside the glomerular capillaries to force the fluid out.
This is where the afferent and efferent arterioles work together like a precision-engineered system. Because the afferent arteriole is wider than the efferent arteriole, blood can enter the glomerulus more easily than it can leave. This creates a "traffic jam" of blood inside the glomerulus, building up the pressure needed for filtration. Think of it like partially blocking the end of a garden hose with your thumb; the water pressure inside the hose increases, forcing the water out with more speed.
If the afferent arteriole constricts (narrows), less blood flows in, and the pressure in the glomerulus drops, leading to less filtration. If it dilates (widens), more blood flows in, increasing the pressure and resulting in more filtration.
The Body's Built-in Thermostat: Autoregulation
Your blood pressure changes throughout the day. When you run, it goes up; when you sleep, it goes down. If the pressure in the glomerulus changed that much, your kidneys would either filter too much or too little, which would be disastrous for the body's internal balance. Thankfully, the afferent arteriole has a special ability called autoregulation.
Autoregulation is the process by which the afferent arteriole automatically adjusts its diameter to maintain a constant glomerular filtration rate (GFR)[1], even when your overall blood pressure changes.
For example:
- If your blood pressure rises, the smooth muscle cells in the wall of the afferent arteriole are stretched. They respond by constricting. This narrows the entrance, reducing blood flow into the glomerulus and preventing a dangerous rise in filtration pressure.
- If your blood pressure falls, the stretch on the afferent arteriole decreases. It responds by dilating. This widens the entrance, allowing more blood to flow in and maintaining a stable filtration pressure.
This is similar to a thermostat in your house. If the room gets too cold, the heater turns on. If it gets too hot, the heater turns off. The afferent arteriole is the kidney's thermostat for blood pressure.
A Real-World Scenario: Regulating Blood Pressure
Let's follow a concrete example to see how the afferent arteriole works in a real-life situation.
Scenario: You decide to stand up very quickly after lying on the couch for an hour. Gravity pulls blood down to your legs, causing a momentary drop in the blood pressure reaching your brain and your kidneys.
Step 1: The drop in blood pressure is detected by the juxtaglomerular (JG) cells[2], which are specialized cells located in the walls of the afferent arteriole.
Step 2: The JG cells interpret the low pressure as a signal that the body needs to conserve fluid and increase pressure. They release an enzyme called renin into the bloodstream.
Step 3: Renin triggers a series of chemical reactions (the Renin-Angiotensin-Aldosterone System, or RAAS[3]) that ultimately result in two key actions:
- Widespread constriction of blood vessels throughout the body, raising blood pressure.
- Constriction of the efferent arteriole. This is a clever backup plan. By narrowing the exit, pressure builds up inside the glomerulus even with less blood coming in, helping to preserve the GFR.
Step 4: At the same time, the afferent arteriole itself dilates due to the autoregulation mechanism described earlier, allowing as much blood as possible to enter the glomerulus.
Outcome: Through the coordinated actions of the afferent and efferent arterioles, your kidneys maintain a stable filtration rate, and your body quickly restores normal blood pressure, preventing you from feeling dizzy.
Important Questions
What happens if the afferent arteriole is blocked or damaged?
How do medications like ACE inhibitors affect the afferent arteriole?
Why is the afferent arteriole's role so critical during exercise?
Footnote
[1] GFR (Glomerular Filtration Rate): The volume of fluid filtered from the glomerular capillaries into the Bowman's capsule per unit time. It is a key measure of kidney function.
[2] Juxtaglomerular (JG) Cells: Specialized smooth muscle cells located mainly in the wall of the afferent arteriole that synthesize, store, and release the enzyme renin.
[3] RAAS (Renin-Angiotensin-Aldosterone System): A hormone system that regulates blood pressure and fluid balance. Renin from the JG cells starts this cascade.