Oxyhemoglobin: The Oxygen-Carrying Molecule
What is Hemoglobin? The Oxygen Taxi Service
Before we dive into oxyhemoglobin, we need to understand its foundation: hemoglobin. Imagine your bloodstream as a massive, complex highway system. The cargo that every single cell needs to survive is oxygen. But oxygen doesn't dissolve well in blood plasma (the liquid part of blood). It would be like trying to deliver packages by just tossing them into a river—highly inefficient!
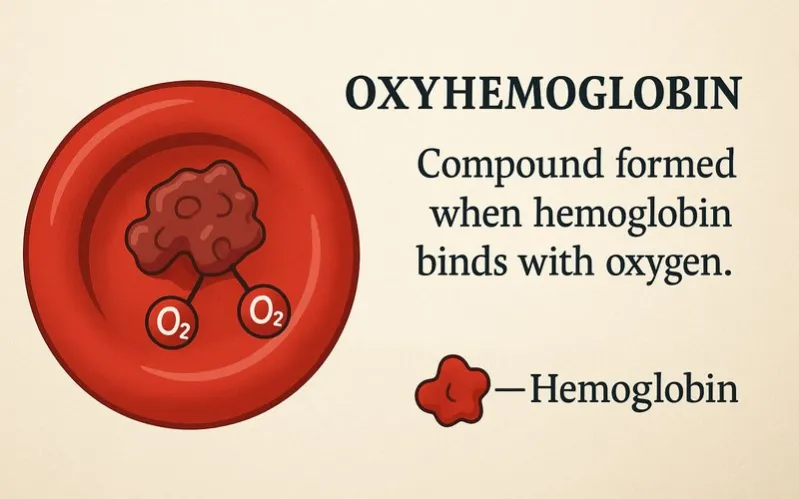
This is where hemoglobin comes in. Think of hemoglobin as a fleet of microscopic taxis or delivery trucks specifically designed to pick up and carry oxygen. Hemoglobin ($ Hb $) is a large, complex protein found inside red blood cells[1]. Each hemoglobin molecule is made up of four parts, or subunits. Each subunit contains a heme group, which is the actual "passenger seat" for oxygen.
The heme group has a single iron atom ($ Fe $) at its center. This iron atom is the key player because it can bind to an oxygen molecule ($ O_2 $). Since there are four heme groups in one hemoglobin molecule, each taxi can carry up to four oxygen passengers at a time.
The Formation of Oxyhemoglobin: Picking Up Passengers
The process of hemoglobin binding with oxygen is called oxygenation. When this happens, the resulting compound is called oxyhemoglobin ($ HbO_2 $). This chemical reaction can be written as a simple formula:
$ Hb + O_2 \rightleftharpoons HbO_2 $
The double arrow ($ \rightleftharpoons $) is crucial. It means the reaction is reversible. Oxyhemoglobin is formed in the lungs, where oxygen levels are high. But it can also break apart (dissociate) in body tissues, where oxygen levels are low, releasing its precious cargo.
Why does this happen? It's all about concentration. In the capillaries[2] of the lungs, the concentration of oxygen is very high. Oxygen diffuses from the air sacs (alveoli[3]) into the blood and readily binds to the iron in hemoglobin, forming bright red oxyhemoglobin. This is why arterial blood[4], carrying oxygen away from the heart and lungs, is bright red.
The Oxygen Dissociation Curve: The Delivery Schedule
How does our body control when and where oxygen is dropped off? This is explained by the oxygen-hemoglobin dissociation curve. This graph shows the relationship between the partial pressure of oxygen (a measure of oxygen concentration) and the percentage of hemoglobin that is saturated with oxygen (i.e., converted to oxyhemoglobin).
The curve has a distinctive S-shape (sigmoidal shape). This shape is incredibly important:
- In the Lungs (High $ O_2 $ Pressure): The top part of the curve is flat. This means that even if the oxygen pressure drops a little in the lungs (like when you're at a high altitude), hemoglobin can still become almost fully saturated with oxygen. It's a safety buffer.
- In the Tissues (Low $ O_2 $ Pressure): The steep part of the curve shows that a small drop in oxygen pressure causes a large amount of oxygen to be unloaded from oxyhemoglobin. This ensures that active tissues, which are using up oxygen quickly, get the supply they need.
Several factors can shift this curve, making it easier or harder for oxygen to be released. For example, higher acidity (lower pH), higher carbon dioxide levels, and higher temperature—all conditions found in active muscles—shift the curve to the right, promoting oxygen release exactly where it's needed most.
| Factor | Condition (e.g., in Active Muscle) | Effect on Curve | Result |
|---|---|---|---|
| Acidity (pH) | Decreases (more acidic) | Shifts Right | Oxygen is released more easily |
| Carbon Dioxide ($ CO_2 $) | Increases | Shifts Right | Oxygen is released more easily |
| Temperature | Increases | Shifts Right | Oxygen is released more easily |
| 2,3-DPG[5] (a compound in RBCs) | Increases (e.g., at high altitude) | Shifts Right | Oxygen is released more easily |
Oxyhemoglobin in Action: From a Sprint to a Mountain Climb
Let's see how oxyhemoglobin works in real-life situations.
Example 1: Running a Race
When you start sprinting, your leg muscles work frantically. They burn energy, consuming oxygen and producing carbon dioxide and acid (lactic acid) as waste. This creates the perfect conditions for oxygen delivery: the muscle tissue becomes warmer, more acidic, and has higher $ CO_2 $ levels. As your oxygen-rich blood flows through these muscles, these conditions cause the oxyhemoglobin to destabilize, shifting the dissociation curve to the right and forcing it to unload more oxygen than it would in a resting muscle. Your hard-working cells get the fuel they need, thanks to this clever mechanism.
Example 2: Adapting to High Altitude
At the top of a high mountain, the air is "thinner," meaning there is less oxygen pressure. When you first arrive, your body might struggle to fully saturate hemoglobin with oxygen. In response, your body produces more red blood cells and more 2,3-DPG inside them. The increased 2,3-DPG shifts the oxygen dissociation curve to the right, helping to unload oxygen more effectively in your tissues, even though the initial oxygen pickup in the lungs was slightly harder. This is a fantastic example of the body's ability to adapt.
Common Mistakes and Important Questions
A: Not exactly. This is a common mix-up. Oxyhemoglobin refers specifically to the hemoglobin molecule that is bound to oxygen. Oxygenated blood is the blood that contains a high percentage of oxyhemoglobin. So, oxyhemoglobin is the compound, and oxygenated blood is the mixture containing that compound.
A: Oxyhemoglobin ($ HbO_2 $) is hemoglobin with oxygen attached. It is bright red. Deoxyhemoglobin is hemoglobin that has released its oxygen. It is a darker, purplish-red color. This color difference is why arterial blood (high in oxyhemoglobin) is bright red and venous blood (high in deoxyhemoglobin) is dark red.
A: Yes, and this can be dangerous. Carbon monoxide ($ CO $) is a gas that binds to the iron in hemoglobin over 200 times more tightly than oxygen does. When it binds, it forms carboxyhemoglobin. This prevents oxygen from binding, starving the body's tissues of oxygen, which can lead to poisoning and even death.
Footnote
[1] Red Blood Cells (RBCs or Erythrocytes): The most common type of blood cell, whose main function is to carry oxygen from the lungs to the body tissues.
[2] Capillaries: The smallest blood vessels where the exchange of water, oxygen, carbon dioxide, and other substances between blood and tissues occurs.
[3] Alveoli (singular: Alveolus): Tiny air sacs in the lungs where the exchange of oxygen and carbon dioxide takes place.
[4] Arterial Blood: Blood that is pumped from the heart to the rest of the body, typically rich in oxygen.
[5] 2,3-DPG (2,3-Diphosphoglycerate): A substance found in red blood cells that affects the affinity of hemoglobin for oxygen. Higher levels make hemoglobin release oxygen more easily.