The Respiratory System: Your Body's Life-Sustaining Engine
The Pathway of a Breath: A Journey Through the Respiratory Tract
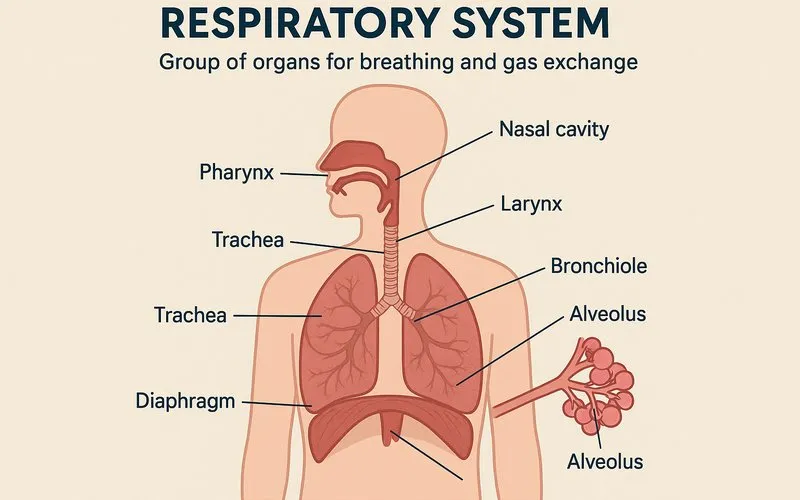
Every breath you take starts a remarkable journey. The respiratory tract is like a sophisticated, branching tunnel system designed to prepare air for your lungs. It is divided into two main parts: the upper and lower respiratory tracts.
| Section | Organs/Structures | Primary Function |
|---|---|---|
| Upper Respiratory Tract | Nose, Nasal Cavity, Pharynx (Throat), Larynx (Voice Box) | Filtering, warming, and humidifying inhaled air; smell; sound production. |
| Lower Respiratory Tract | Trachea (Windpipe), Bronchi, Bronchioles, Lungs, Alveoli | Conducting air to the lungs; site of gas exchange (O2 and CO2). |
Imagine breathing in cold, dry winter air. Your nose acts as a climate control system. The tiny hairs (vibrissae) and mucus trap dust and germs, while the rich blood supply in the nasal passages warms the air to body temperature. The air then travels down the pharynx, a shared passage for air and food, and enters the larynx. The larynx contains your vocal cords, which vibrate as air passes through to create sound. A small flap called the epiglottis acts like a trapdoor, closing over the larynx when you swallow to prevent food from "going down the wrong pipe."
The air then enters the trachea, a tube reinforced with C-shaped rings of cartilage that keep it from collapsing. At its base, the trachea splits into two tubes called the primary bronchi (singular: bronchus), one leading to each lung. Inside the lungs, the bronchi branch out like a tree into smaller bronchioles. The smallest bronchioles, called terminal bronchioles, end in tiny air sacs called alveoli (singular: alveolus). This is where the real magic of gas exchange happens.
The Mechanics of Breathing: Inhalation and Exhalation
Breathing, or pulmonary ventilation, is a mechanical process driven by pressure changes. It involves two main phases: inhalation (breathing in) and exhalation (breathing out).
Inhalation is an active process. It requires the contraction of key muscles. The primary muscle is the diaphragm, a large, dome-shaped muscle located at the bottom of the chest cavity. When it contracts, it flattens and moves downward. At the same time, the external intercostal muscles between your ribs contract, lifting your rib cage upward and outward. These actions increase the volume of the thoracic cavity. Because the lungs are stuck to the chest wall by a thin layer of fluid, they expand too. As lung volume increases, the air pressure inside them falls below the air pressure outside your body. Air naturally flows from high pressure to low pressure, so it rushes into your nose and down into your lungs.
Exhalation is usually a passive process. During quiet breathing, you don't need to use any energy to breathe out. You simply relax your diaphragm and intercostal muscles. The diaphragm returns to its dome shape, and the rib cage drops down and inward. This decreases the volume of the thoracic cavity, which increases the pressure inside the lungs above atmospheric pressure. The higher-pressure air is then pushed out. However, during forceful exhalation (like blowing out candles), it becomes an active process involving abdominal and other internal muscles.
The Miracle of Gas Exchange: From Air to Blood
The final destination of inhaled air is the alveoli. These are microscopic, grape-like clusters at the end of the bronchial tree. Each lung contains hundreds of millions of alveoli, providing a massive surface area for gas exchange—roughly the size of a tennis court!
Each alveolus is surrounded by a network of tiny blood vessels called capillaries. The wall of the alveolus and the wall of the capillary are extremely thin, together forming the respiratory membrane. This setup is perfect for diffusion, the movement of molecules from an area of high concentration to an area of low concentration.
Here's how it works step-by-step:
- After inhalation, the air in the alveoli has a high concentration of oxygen (O2) and a low concentration of carbon dioxide (CO2).
- The blood arriving in the capillaries has just returned from the body's tissues. It is deoxygenated, meaning it has a low concentration of O2 and a high concentration of CO2 (a waste product of cellular respiration).
- Due to the difference in concentration, O2 diffuses out of the alveolus, across the respiratory membrane, and into the blood in the capillary.
- Simultaneously, CO2 diffuses out of the blood, across the membrane, and into the alveolus.
- The blood is now oxygenated and returns to the heart to be pumped to the rest of the body. The CO2 in the alveolus is then exhaled out of the body.
This entire process is incredibly efficient and happens in the blink of an eye.
How Oxygen and Carbon Dioxide Travel in the Blood
Gases need a way to be carried in the bloodstream. They do this in two main ways: dissolved directly in the blood plasma or chemically bonded to other molecules.
Oxygen Transport: Only a very small amount (1.5%) of oxygen dissolves directly in plasma. The vast majority (98.5%) is carried by hemoglobin, a protein inside red blood cells. Hemoglobin contains iron, which oxygen binds to, forming oxyhemoglobin. This can be represented by the equation: Hb + O2 ⇋ HbO2. This reaction is reversible; in the body's tissues where oxygen concentration is low, hemoglobin readily releases its oxygen.
Carbon Dioxide Transport: Carbon dioxide is transported in three forms:
- Dissolved in Plasma (7-10%): A small amount dissolves directly.
- Bound to Hemoglobin (20%): CO2 binds to a different part of the hemoglobin molecule than oxygen, forming carbaminohemoglobin.
- As Bicarbonate Ions (70%): This is the most common method. CO2 reacts with water in the red blood cells to form carbonic acid (H2CO3), which quickly breaks down into a hydrogen ion (H+) and a bicarbonate ion (HCO3-). The bicarbonate ion moves out into the plasma for transport. This reaction is reversed in the lungs to release CO2 for exhalation. The chemical formula is: CO2 + H2O ⇋ H2CO3 ⇋ H+ + HCO3-.
Respiratory System in Action: From Exercise to Altitude
The respiratory system is dynamic and responds instantly to the body's needs. A perfect example is what happens during exercise.
When you start running, your muscle cells work harder and need more energy. To produce this energy, they use more oxygen and produce more carbon dioxide. The increased level of CO2 in your blood is detected by special sensors in the brain and major blood vessels. These sensors send signals to the respiratory center in your brainstem to increase the rate and depth of your breathing. This is why you start to pant. Your diaphragm and intercostal muscles contract more forcefully and frequently, drawing more air into your lungs with each breath. This increased ventilation ensures that more oxygen is delivered to the blood and more carbon dioxide is removed, meeting the demands of your active muscles.
Another fascinating application is how the body adapts to high altitudes. At high elevations, the air is "thinner," meaning it has less oxygen. When a person ascends a mountain, their body initially struggles to get enough oxygen. In response, the respiratory rate increases. Over time, the body produces more red blood cells to carry oxygen more efficiently. This is why athletes often train at high altitudes—to naturally boost their red blood cell count and enhance their endurance.
Common Mistakes and Important Questions
Footnote
1 ATP (Adenosine Triphosphate): The primary energy currency of the cell. It provides energy for almost all cellular processes.
2 Alveoli: Tiny, balloon-like air sacs in the lungs where the exchange of oxygen and carbon dioxide takes place.
3 Hemoglobin: An iron-containing protein in red blood cells that binds to oxygen and carbon dioxide for transport.
4 Diaphragm: The primary muscle of respiration, a dome-shaped sheet of muscle that separates the thoracic cavity from the abdominal cavity.
5 Diffusion: The passive movement of molecules or particles from an area of higher concentration to an area of lower concentration.