Air Sacs: The Tiny Powerhouses of Breathing
What Exactly is an Air Sac?
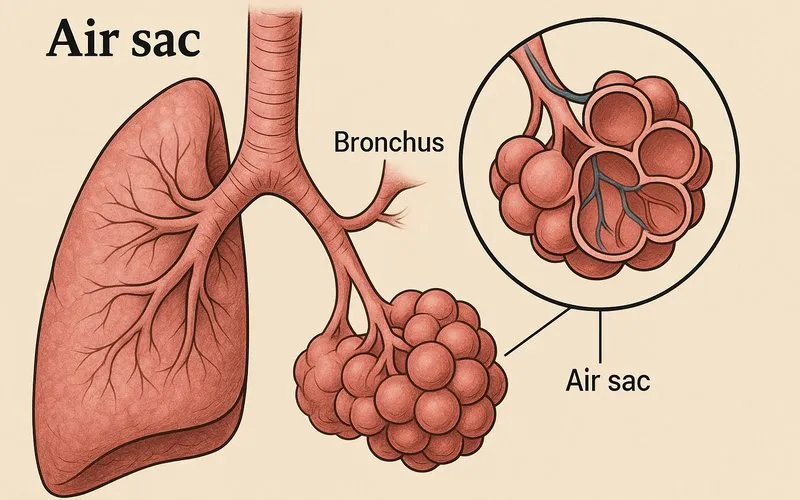
Imagine your lungs as an upside-down tree. The windpipe (trachea) is the trunk. This trunk splits into two large branches (the bronchi), one for each lung. These branches then divide into smaller and smaller twigs (bronchioles). At the very end of the tiniest twigs, you find not leaves, but millions of microscopic, grape-like clusters. Each individual "grape" in this cluster is an air sac, or alveolus.
To understand their scale, consider this: if you could lay all the air sacs from a single human lung flat on the ground, they would cover an area about the size of a tennis court (70-100 square meters)! This enormous surface area is packed into your chest because the air sacs are so incredibly small. Each one has a diameter of about 200-300 micrometers. To put that in perspective, a pinhead is about 1,500 micrometers across. You have roughly 300-500 million alveoli in your lungs.
| Feature | Description | Analogy |
|---|---|---|
| Shape | Tiny, hollow, balloon-like or grape-like cavity. | A cluster of balloons or a bunch of grapes. |
| Size | Diameter of 200-300 μm (micrometers). | About the size of a grain of fine sand. |
| Quantity | 300-500 million per lung. | More than the entire human population of North America. |
| Total Surface Area | 70-100 m² (square meters). | About half a badminton court or a large apartment floor. |
The Marvelous Design for Gas Exchange
The primary job of the air sac is gas exchange. This process is efficient because of three brilliant design features:
1. Thin Walls: The walls of the alveoli are incredibly thin, often only one cell thick. Surrounding each air sac is a network of tiny blood vessels called capillaries[1]. The wall of the alveolus and the wall of the capillary together form a super-thin membrane. Oxygen and carbon dioxide can easily pass through this membrane. It's like two sheets of plastic wrap pressed together – gases can slip right through.
2. Moist Lining: The inner surface of the air sacs is coated with a thin layer of moisture. Gases like oxygen and carbon dioxide must be dissolved in water to diffuse across the membrane. This moisture is essential for gas exchange to happen. You can think of it as needing to dissolve sugar in water before it can spread evenly; the gases need to be "dissolved" to move.
3. Massive Surface Area: As mentioned before, the collective surface area of all the air sacs is huge. This provides a vast "trading floor" where oxygen can enter the blood and carbon dioxide can leave it simultaneously. Without this large area, gas exchange would be slow and inefficient, unable to support an active body.
A Closer Look at the Respiratory Membrane
The barrier where gas exchange occurs is called the respiratory membrane. It's not a single layer but a sandwich of three very thin layers:
- The wall of the alveolus (one cell thick).
- The wall of the capillary (also one cell thick).
- A fused basement membrane[3] between them that acts like a glue.
The total thickness of this membrane is about 0.5 micrometers. This extreme thinness is crucial for rapid gas exchange. The blood cell (red blood cell[4]) actually squeezes through the capillary, pressing up against this membrane, which minimizes the distance the oxygen molecule has to travel. The entire exchange happens in less than a second as the blood cell passes by.
The Role of Surfactant: A Life-Saving Soap
If the alveoli were simple, water-lined balloons, they would have a big problem: the force of surface tension. Water molecules are attracted to each other, which makes the surface of water act like a thin, elastic skin. This force would cause small alveoli to collapse easily, making it very hard to re-inflate them.
To prevent this, special cells in the alveolar walls secrete a substance called pulmonary surfactant[5]. Surfactant is a detergent-like substance that disrupts the water molecules' attraction, reducing surface tension. Think of it like soap in water. Soap makes it easier to blow bubbles because it reduces the surface tension. Similarly, surfactant makes it easier for your alveoli to inflate with each breath.
This is especially critical for newborn babies. Babies born prematurely often struggle to breathe because their bodies haven't started producing enough surfactant yet. This condition is called Respiratory Distress Syndrome (RDS), and it is treated by giving the baby artificial surfactant.
From Breath to Bloodstream: A Step-by-Step Journey
Let's follow an oxygen molecule on its journey from the air to your muscle cells, and a carbon dioxide molecule on its way out.
Oxygen's Path In:
- You inhale air containing oxygen (O$_2$).
- The air travels down your trachea, through the bronchi, and into the bronchioles.
- It finally reaches the alveoli (air sacs).
- The oxygen dissolves in the moist lining of the alveolus.
- It then diffuses across the thin respiratory membrane into the capillary.
- Inside the capillary, it binds to hemoglobin[6], a protein in red blood cells.
- The heart pumps this oxygen-rich blood to every part of your body.
Carbon Dioxide's Path Out:
- Your body's cells produce carbon dioxide (CO$_2$) as a waste product.
- CO$_2$ diffuses from the cells into the blood plasma and red blood cells.
- The heart pumps this carbon dioxide-rich blood back to the lungs.
- In the lung capillaries surrounding the alveoli, CO$_2$ diffuses out of the blood, across the respiratory membrane, and into the air sac.
- You then exhale, releasing the CO$_2$ into the atmosphere.
How Exercise Tests Your Air Sacs
When you are sitting still, only about one-third of your alveoli are actively involved in gas exchange. But when you start running or playing sports, your body's demand for oxygen skyrockets. To meet this demand, your body takes several actions:
- You breathe faster and deeper: This pulls more air into the lungs, inflating more alveoli and bringing fresh oxygen to a larger surface area.
- Your heart beats faster: This pumps blood through the lung capillaries more quickly, so more red blood cells can pick up oxygen and drop off carbon dioxide per minute.
- Blood flow is redirected: More blood is sent to the working muscles and, importantly, to the lungs to maximize gas exchange.
This incredible coordination ensures that even during intense exercise, your air sacs can keep up with your body's energy needs. Regular exercise can even improve the efficiency of your respiratory system over time.
Common Mistakes and Important Questions
A: Yes, they are. "Alveolus" is the precise scientific term (from Latin, meaning "small cavity"), while "air sac" is a common, descriptive name. They refer to the exact same structure.
A: This is a great question! They are prevented from collapsing completely by two main factors. First, the pulmonary surfactant we discussed greatly reduces the surface tension that would cause collapse. Second, there is always a small amount of air left in the lungs after you exhale normally, which helps to keep the alveoli open.
A: The number of alveoli you have is mostly determined by childhood and adolescence. After your lungs are fully developed, you generally do not grow new air sacs. However, the capacity and efficiency of your existing alveoli can be improved with regular cardiovascular exercise. In cases of lung disease where air sacs are destroyed, they cannot be regenerated.
When Things Go Wrong: Diseases Affecting Air Sacs
The delicate structure of alveoli makes them vulnerable to damage from diseases and pollutants. Two major diseases directly target these tiny structures:
Pneumonia: This is an infection that causes inflammation in the alveoli. The air sacs fill with fluid and pus (a thick liquid containing bacteria, white blood cells, and dead tissue), making it difficult to breathe and severely impairing gas exchange. It can be caused by bacteria, viruses, or fungi.
Emphysema (a type of COPD[7]): This is a long-term, progressive disease often caused by smoking. In emphysema, the walls of the alveoli are destroyed. The small, numerous air sacs merge into larger, fewer, and less efficient sacs. This drastically reduces the surface area available for gas exchange, causing severe shortness of breath. The lungs also lose their elasticity, making exhalation difficult.
Footnote
[1] Capillaries: The smallest blood vessels in the body, connecting arteries and veins. Their thin walls allow for the exchange of substances like oxygen and carbon dioxide between blood and tissues.
[2] Diffusion: The passive movement of molecules or particles from a region of higher concentration to a region of lower concentration.
[3] Basement Membrane: A thin, fibrous layer that provides support and helps attach epithelial cells (like those lining the alveolus) to underlying tissues.
[4] Red Blood Cell (Erythrocyte): A cell in the blood that contains hemoglobin and is responsible for carrying oxygen from the lungs to the body's tissues.
[5] Pulmonary Surfactant: A fluid secreted by the alveoli that reduces surface tension, preventing the air sacs from collapsing. (Pulmonary means "related to the lungs.")
[6] Hemoglobin: An iron-containing protein in red blood cells that binds to oxygen molecules, allowing the blood to transport oxygen.
[7] COPD (Chronic Obstructive Pulmonary Disease): A group of lung diseases that block airflow and make it difficult to breathe. Emphysema and chronic bronchitis are the most common.